Abstract
Introduction: Trace metals play a critical role in human physiology and pathology. Deficiencies or toxicities in trace metals are associated with hematologic abnormalities and disorders and are included in the investigation of some hematology patients. For example, lead, copper and zinc levels may be included in the work-up of patients with unexplained anemia. The practice and clinical utility of these trace metal testing in unselected patients referred to hematology, however, are not well described. We examined the current practice of trace metal testing including lead, copper, and zinc, in hematology patients at a single tertiary care centre with the goal of informing future laboratory utilization of these investigations by hematologists.
Methods: We investigated all adult patients who underwent trace metal testing ordered by hematologists between January 1, 2017, to December 31, 2021, at London Health Science Centre in London, Ontario, Canada. A retrospective chart review was performed to extract clinical and laboratory data including lead (whole blood), copper (plasma) and zinc (plasma) levels. Abnormal trace metal results were defined based on standard laboratory reference ranges. Primary outcomes were indications for trace metal testing and frequency of abnormal tests. Secondary outcomes included associated occupational exposures and clinical utility of testing, defined as the proportion of patients with an abnormal result that impacted diagnosis or management (including interventions such as advice to reduce exposures or initiate treatment such as chelation therapy or supplementation).
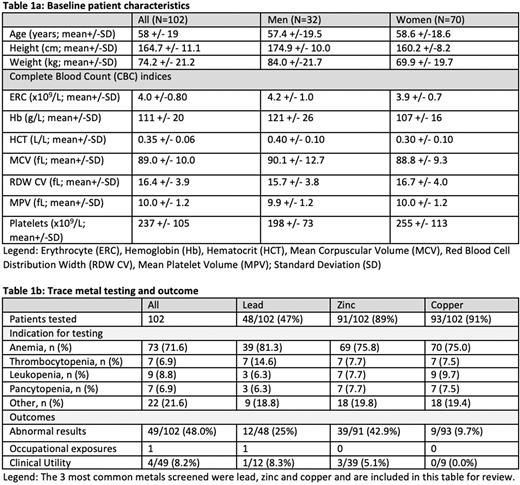
Results: Preliminary results on 102/189 patients within our defined cohort revealed mean age 58 years with 32 men and 70 women tested for trace metals (Table 1a). Common indications for testing of each metal included work up for cytopenias, most commonly anemia (Table 1b). The three most common trace metals tested were 48/102 (47%) lead, 91/102 (89%) zinc, and 93/102 (91%) copper. Abnormal results were identified in 49 (48%) of the 102 patients with 12/48 (25%) in lead, 39/91 (42.9%) in zinc, and 9/93 (9.7%) copper testing. For lead, all abnormal results were toxicities, all abnormal results for zinc were deficiencies, and abnormal results for copper had a mix of both deficiencies and toxicities. Clinical utility was identified in one patient (8.3%) with an abnormal lead level, three (5.1%) with abnormal zinc levels, but none in the copper group. The single occupational exposure identified was toxic lead (greater than 50 times the upper limit of normal) in a patient with normal blood counts who made lead bullets. Data analysis for the full cohort is in progress and will be presented in the future.
Conclusion: In this single-centre retrospective study, we characterized the use of trace metal testing for lead, zinc and copper deficiencies and toxicities by hematologists. Abnormal levels in these three metals are relatively common (48% for the entire cohort) with the highest frequency in zinc (43%) and lead (25%). However, despite the identification of abnormal results, clinical utility was low as management of patients with abnormal levels were not affected. This may indicate that the level of abnormality was trivial and did not require intervention in the majority of these identified. With this preliminary data, we speculate that some trace metal testing may be ordered as a non-specific panel of laboratory investigations for various indications and slightly abnormal results do not lead to any change in clinical management. Further investigations to explore the degree of trace metal level abnormalities and the impact on clinical diagnosis and management in these hematology patients are underway. The role of trace metal testing, the relationship between abnormal trace metal results and cytopenias such as anemia and impact on management will help to inform future clinical practice in hematology.
Disclosures
Hsia:Medison: Consultancy, Honoraria, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal